Antimicrobial resistance and prevalence of Staphylococcus aureus in veterinary sources in south Brazil, 2017–2023
Resumo
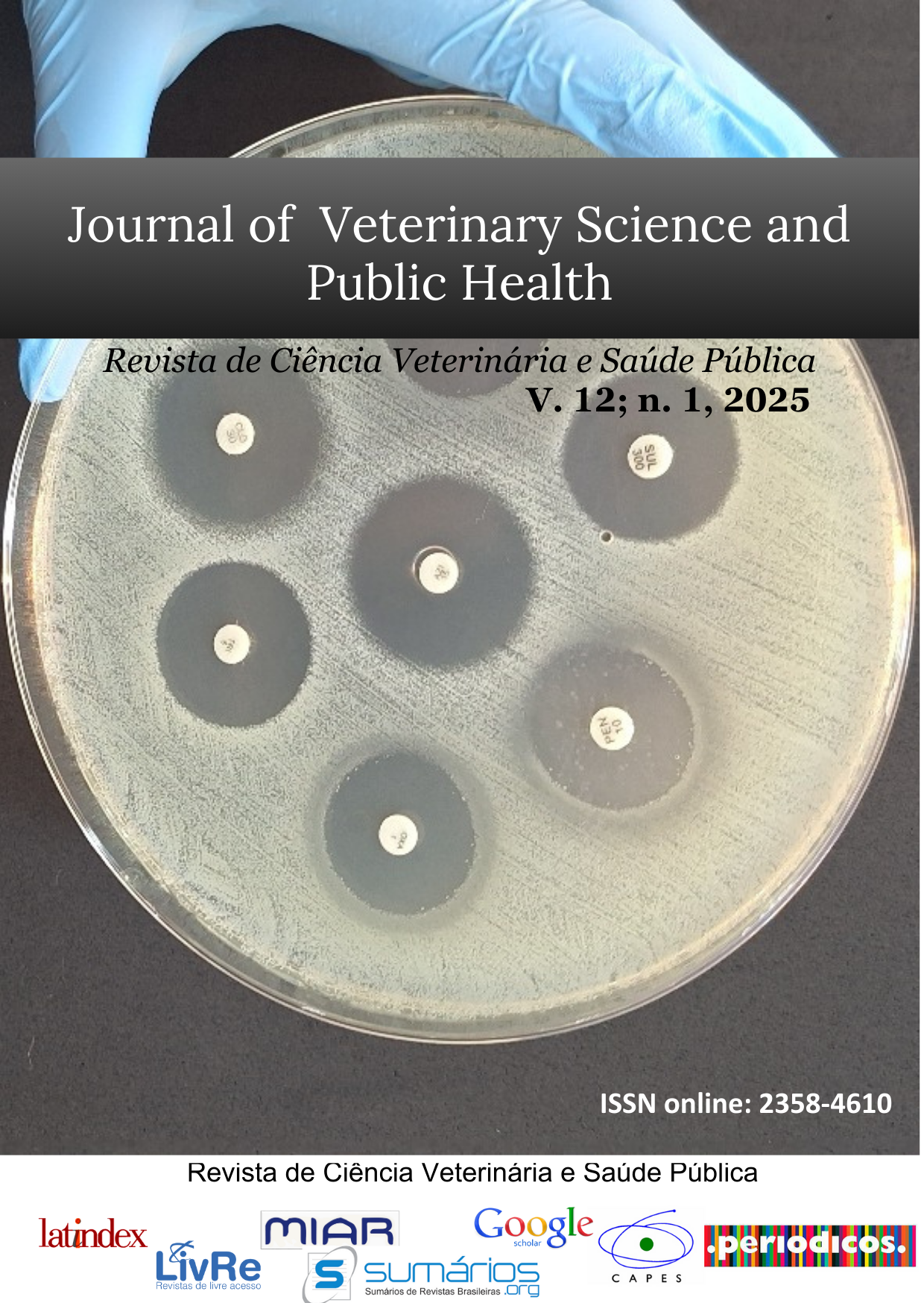
Surveillance studies are essential for tracking the emergence and spread of antimicrobial resistance, which can help identify the most effective strategies for international stewardship in containing the spread of resistant infections. This study investigated the prevalence and resistance patterns of Staphylococcus aureus in southern Brazil from 2017 to 2023. A total of 3,435 clinical specimens were collected from veterinary sources and tested for Staphylococcus aureus. Antibiotic susceptibility testing was performed using the disc diffusion method, and a new categorization of antibiotics based on resistance levels was proposed. The results showed that Staphylococcus aureus isolates exhibited high resistance to various commonly prescribed antibiotics, with significant differences among antibiotic classes. Multidrug resistance showed temporal variations, with a peak of 54.29% in 2021. The study suggested that empirical treatment guidelines may need revision, and regional variations in antimicrobial resistance rates should be considered. These results also highlight the dynamic nature of antimicrobial resistance and indicate the need for continuous surveillance and rational use of antibiotics to prevent the dissemination of resistant strains of Staphylococcus aureus from veterinary sources.
Downloads
Referências
Agency, E. M. (2019). European Surveillance of Veterinary Antimicrobial Consumption (ESVAC).
Chokshi, A., Sifri, Z., Cennimo, D., & Horng, H. (2019). Global Contributors to Antibiotic Resistance. J Glob Infect Dis, 11(1), 36-42. doi:10.4103/jgid.jgid_110_18
Clarke, H. T. (2015). Chemistry of penicillin (Vol. 2167): Princeton University Press.
Clinical, & Institute, L. S. (2015). Performance Standards for Antimicrobial Disk Susceptibility Tests for Bacteria Isolated from Animals: CLSI Supplement VET01S; Replaces VET01-S2: Clinical and Laboratory Standards Institute.
David, M. Z., & Daum, R. S. (2017). Treatment of Staphylococcus aureus Infections. In F. Bagnoli, R. Rappuoli, & G. Grandi (Eds.), Staphylococcus aureus: Microbiology, Pathology, Immunology, Therapy and Prophylaxis (pp. 325-383). Cham: Springer International Publishing.
Deurenberg, R. H., Vink, C., Kalenic, S., Friedrich, A. W., Bruggeman, C. A., & Stobberingh, E. E. (2007). The molecular evolution of methicillin-resistant Staphylococcus aureus. Clin Microbiol Infect, 13(3), 222-235. doi:10.1111/j.1469-0691.2006.01573.x
Deyno, S., Fekadu, S., & Astatkie, A. (2017). Resistance of Staphylococcus aureus to antimicrobial agents in Ethiopia: a meta-analysis. Antimicrob Resist Infect Control, 6(1), 85. doi:10.1186/s13756-017-0243-7
El Omeiri, N., Beith, A., Bruinsma, N., Caipo, M., Barcos, L., Mesplet, M., . . . Ramon-Pardo, P. (2023). Driving multisectoral antimicrobial resistance action in South America: Lessons learned from implementing an enhanced tripartite AMR country self-assessment tool. One Health, 16, 100474. doi:https://doi.org/10.1016/j.onehlt.2022.100474
Food, & Administration, D. (2018). Supporting antimicrobial stewardship in veterinary settings. In: Issue September.
Ge, B., Mukherjee, S., Hsu, C. H., Davis, J. A., Tran, T. T. T., Yang, Q., . . . McDermott, P. F. (2017). MRSA and multidrug-resistant Staphylococcus aureus in U.S. retail meats, 2010-2011. Food Microbiol, 62, 289-297. doi:10.1016/j.fm.2016.10.029
Hodiamont, C. J., van den Broek, A. K., de Vroom, S. L., Prins, J. M., Mathot, R. A. A., & van Hest, R. M. (2022). Clinical Pharmacokinetics of Gentamicin in Various Patient Populations and Consequences for Optimal Dosing for Gram-Negative Infections: An Updated Review. Clin Pharmacokinet, 61(8), 1075-1094. doi:10.1007/s40262-022-01143-0
Jfoster, T. (2002). Staphylococcus aureus. In M. Sussman (Ed.), Molecular Medical Microbiology (pp. 839-888). London: Academic Press.
Lancette, G. A., Peeler, J. T., & Lanier, J. M. (2020). Evaluation of an Improved MPN Medium for Recovery of Stressed and Nonstressed Staphylococcus aureus. Journal of Association of Official Analytical Chemists, 69(1), 44-46. doi:10.1093/jaoac/69.1.44 %J Journal of Association of Official Analytical Chemists
Levandowski, R., Daroit, L., & dos Santos, L. R. (2019). Escherichia coli: Antimicrobial susceptibility monitoring 2015–2018 in Brazil. Revista de Ciência Veterinária e Saúde Pública, 6(2), 251-261.
Marston, H. D., Dixon, D. M., Knisely, J. M., Palmore, T. N., & Fauci, A. S. (2016). Antimicrobial Resistance. JAMA, 316(11), 1193-1204. doi:10.1001/jama.2016.11764
Medina, M.-j., Legido-Quigley, H., & Hsu, L. Y. (2020). Antimicrobial Resistance in One Health. In A. J. Masys, R. Izurieta, & M. Reina Ortiz (Eds.), Global Health Security (pp. 209-229). Cham: Springer International Publishing.
Michael, C. A., Dominey-Howes, D., & Labbate, M. (2014). The antimicrobial resistance crisis: causes, consequences, and management. Front Public Health, 2, 145. doi:10.3389/fpubh.2014.00145
Neyra, R. C., Frisancho, J. A., Rinsky, J. L., Resnick, C., Carroll, K. C., Rule, A. M., . . . Silbergeld, E. K. (2014). Multidrug-resistant and methicillin-resistant Staphylococcus aureus (MRSA) in hog slaughter and processing plant workers and their community in North Carolina (USA). Environ Health Perspect, 122(5), 471-477. doi:10.1289/ehp.1306741
Pereira, S. G., Marques, M., Pereira, J., & Cardoso, O. (2015). Multidrug and extensive drug resistance in Pseudomonas aeruginosa clinical isolates from a Portuguese central hospital: 10-year survey. Microb Drug Resist, 21(2), 194-200. doi:10.1089/mdr.2014.0137
Salam, M. A., Al-Amin, M. Y., Pawar, J. S., Akhter, N., & Lucy, I. B. (2023). Conventional methods and future trends in antimicrobial susceptibility testing. Saudi J Biol Sci, 30(3), 103582. doi:10.1016/j.sjbs.2023.103582
Scarpellini, R., Assirelli, G., Giunti, M., Esposito, E., Mondo, E., Piva, S., & Khurshid, M. (2023). Monitoring the Prevalence of Antimicrobial Resistance in Companion Animals: Results from Clinical Isolates in an Italian University Veterinary Hospital. Transboundary and Emerging Diseases, 2023, 1-9. doi:10.1155/2023/6695493
Shitandi, A., & Sternesjo, A. (2004). Prevalence of multidrug resistant Staphylococcus aureus in milk from large- and small-scale producers in Kenya. J Dairy Sci, 87(12), 4145-4149. doi:10.3168/jds.S0022-0302(04)73557-2
Silva, W. P. d., Destro, M. T., Landgraf, M., & Franco, B. D. G. M. (2000). Biochemical characteristics of typical and atypical Staphylococcus aureus in mastitic milk and environmental samples of Brazilian dairy farms. Brazilian Journal of Microbiology, 31.
Sweeney, M. T., Lubbers, B. V., Schwarz, S., & Watts, J. L. (2018). Applying definitions for multidrug resistance, extensive drug resistance and pandrug resistance to clinically significant livestock and companion animal bacterial pathogens. J Antimicrob Chemother, 73(6), 1460-1463. doi:10.1093/jac/dky043
Tong, S. Y., Davis, J. S., Eichenberger, E., Holland, T. L., & Fowler, V. G., Jr. (2015). Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev, 28(3), 603-661. doi:10.1128/CMR.00134-14
Turner, N. A., Sharma-Kuinkel, B. K., Maskarinec, S. A., Eichenberger, E. M., Shah, P. P., Carugati, M., . . . Fowler, V. G., Jr. (2019). Methicillin-resistant Staphylococcus aureus: an overview of basic and clinical research. Nat Rev Microbiol, 17(4), 203-218. doi:10.1038/s41579-018-0147-4
van Bijnen, E. M., Paget, J., de Lange-de Klerk, E. S., den Heijer, C. D., Versporten, A., Stobberingh, E. E., . . . collaboration with the, A. S. T. (2015). Antibiotic Exposure and Other Risk Factors for Antimicrobial Resistance in Nasal Commensal Staphylococcus aureus: An Ecological Study in 8 European Countries. PLOS ONE, 10(8), e0135094. doi:10.1371/journal.pone.0135094
Van Boeckel, T. P., Pires, J., Silvester, R., Zhao, C., Song, J., Criscuolo, N. G., . . . Laxminarayan, R. (2019). Global trends in antimicrobial resistance in animals in low- and middle-income countries. Science, 365(6459), eaaw1944. doi:10.1126/science.aaw1944
Wang, S., Zhang, Y., Zhang, X., & Li, J. (2020). An evaluation of multidrug-resistant (MDR) bacteria in patients with urinary stone disease: data from a high-volume stone management center. World J Urol, 38(2), 425-432. doi:10.1007/s00345-019-02772-0
Waters, A. E., Contente-Cuomo, T., Buchhagen, J., Liu, C. M., Watson, L., Pearce, K., . . . Price, L. B. (2011). Multidrug-Resistant Staphylococcus aureus in US Meat and Poultry. Clin Infect Dis, 52(10), 1227-1230. doi:10.1093/cid/cir181
Zhang, J., Wang, J., Jin, J., Li, X., Zhang, H., Shi, X., & Zhao, C. (2022). Prevalence, antibiotic resistance, and enterotoxin genes of Staphylococcus aureus isolated from milk and dairy products worldwide: A systematic review and meta-analysis. Food Res Int, 162(Pt A), 111969. doi:10.1016/j.foodres.2022.111969
Zhang, X., Zhou, Q., Tang, M., Pu, J., Zhang, J., Lu, J., . . . Gao, Y. (2021). Aminoglycoside Resistance and Possible Mechanisms in Campylobacter Spp. Isolated From Chicken and Swine in Jiangsu, China. Front Microbiol, 12, 716185. doi:10.3389/fmicb.2021.716185
Zhang, Y., & Wang, H. (2014). Interpretation of major changes in CLSI M100-S24. Chinese Journal of Laboratory Medicine, 256-260.